Administration processes, paperwork and denial rates are the topmost reasons for Physician burnout. According to a national survey of hospitals, health systems and post-acute care providers conducted by Premier, Inc, nearly 14% of overall claims were initially denied albeit 3.2% of them were pre-approved via prior authorization process and nearly 15% of claims submitted to private payers were also initially denied.
At Falckon Health we help our clients secure their revenue by minimizing the probabilities of running into claim denials. Our practices and recommendations made simple by following these few steps resulting in >80% Clean Claim Rate:
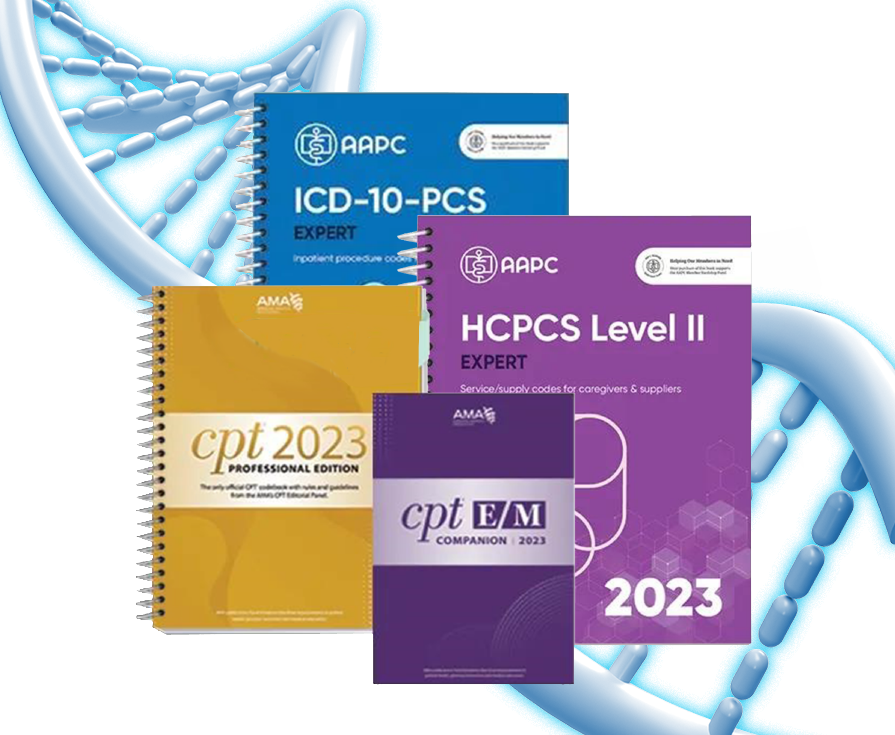
01| Improve Your Coding Accuracy
Healthcare providers can lose about 5% of revenue due to coding errors. In addition, penalties for coding errors such as upcoding, unbundling, duplicate billing, can also get you close to a lump some of penalties. Always make sure to:
- Check and avoid popular coding errors.
- Hire or consult certified professional coders.
- Implement processes in the line to re-check & rectify coding errors before billing and posting.
02| Adjust Your Workflow KPIs for Better Billing & Posting Practices
- Understand the payers’ filing deadlines
- Try to capture the charges and billing within 2days from the Date of Service
- Bill it to the right place
- Try to submit the claim within 3 days from the date of service.
- Try to post the payment within 2days of receiving payments.

03| Use Automation to Prevent Human Errors and Expedite Processing
• Introduce Automation to your workflow especially, for VOB, Posting, and Charge Capturing.
• Automation could be implemented in your systems by using small macros to more complex scripts
• Process automation coupled with manual review can avoid overall errors.

04| Implement Effective VOB techniques
Effective and proper VOB practices not only helps you to avoid initial denial rates but also enhances the patient experience, and relationships with payers. Try to walk your patients through the followings when they initially contact you for the service.
- Eligibility: Get to know the patient’s health insurance plans (Primary/Secondary/Tertiary); Check the coverage is active at the time of services, and understand the overall list of services, treatments, and procedures they are eligible for.
- Patient’s liabilities: Check for deductibles/copays and other financial liabilities that patient may encounter at the time of service and clearly communicate it to the patient.
- Preauthorization: Check for prior authorization requirements for the inquired services, and work it according to the timeline specified by the coverage if any of the services require pre-auth.
- Network Verification: Check for In-network status to be within the coverage levels or inform the patient of lack of coverage if the provider is out-of-network.
- Standardize the procedures:
- Create a checklist for VOB staff to maintain correct procedures.
- Implement a system to keep records of communication or proof of contact.
- Make sure all important details are captured and communicated promptly to patients and payers.

05| Fine Tune Your Credentialing & Contracting Workflow
- Use a centralized credentialing software or update your credentialing platform in a timely manner.
- Conduct regular audits at least once in 6 months.
- Review overall payer contracts & update them every year.

06| Use Analytical tools and insights

07| Update Your Complete RCM Flow Chart
- Review your entire RCM workflow at least once a year or when federal/states regulatory changes, payer contract changes, technology changes occur.
- Include overall staff involvement from billing, IT, compliance, clinic, and finance departments when updating or continuously monitor for updates and changes in these areas if you manage the practice on your own.